Why it matters:
Skin Cancer Statistics
Melanoma
Basal Cell Carcinoma
Melanoma
An estimated 192, 310 new cases of melanoma will be diagnosed in 2019. (1)
An estimated 7,230 people will die of melanoma in 2019. (1)
Men age 49 and under have a higher probability of developing melanoma than any other cancer. (1)
Women age 49 and under are more likely to develop melanoma than any other cancer except breast and thyroid cancers.(1)
Melanomas in blacks, Asians and native Hawaiians most often occur on non-exposed skin with less pigment, with up to 60 to 75 percent of tumors arising on the palms, soles, mucous membranes and nail regions. (2)
Late-stage melanoma diagnoses are more prevalent among Hispanic and black patients than non-Hispanic white patients; 52 percent of non-Hispanic black patients and 26 percent of Hispanic patients receive an initial diagnosis of advanced stage melanoma, versus 16 percent of non-Hispanic white patients. (3)
Cancer Facts and Figures 2019. American Cancer Society. https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures-2019.html. Accessed January 14, 2019.
Gloster HM, Neal K. Skin cancer in skin of color. J Am Acad Dermatol 2006; 55:741-60.
Hu S, Soza-Vento RM, Parker DF, et al. Comparison of stage at diagnosis of melanoma among Hispanic, black, and white patients in Miami-Dade County, Florida. Arch Dermatol 2006; 142(6):704-8.
See more statistics at Skincancer.org
Non-Melanoma
Basal cell carcinoma (BCC) is the most common form of skin cancer. An estimated 4.3 million cases of BCC are diagnosed in the U.S. each year. (1)
Squamous cell carcinoma (SCC) is the second most common form of skin cancer. More than 1 million cases of SCC are diagnosed in the U.S. each year.(1)
The latest figures suggest that more than 15,000 people die of SCC in the U.S. each year—more than twice as many as from melanoma. (2)
Organ transplant patients are approximately 100 times more likely than the general public to develop squamous cell carcinoma. (3)
Rogers HW, Weinstock MA, Feldman SR, Coldiron BM. Incidence estimate of nonmelanoma skin cancer (keratinocyte carcinomas) in the US population, 2012. JAMA Dermatol 2015; 151(10):1081-1086.
Mansouri B, Housewright C. The treatment of actinic keratoses—the rule rather than the exception. J Am Acad Dermatol 2017; 153(11):1200. doi:10.1001/jamadermatol.2017.3395.
Lindelöf B, Sigurgeirsson B, Gäbel H, et al. Incidence of skin cancer in 5356 patients following organ transplantation. Br J Dermatol 2000; 143(3):513-9
See more statistics at Skincancer.org
What to look for:
Tools and techniques for the self evaluation

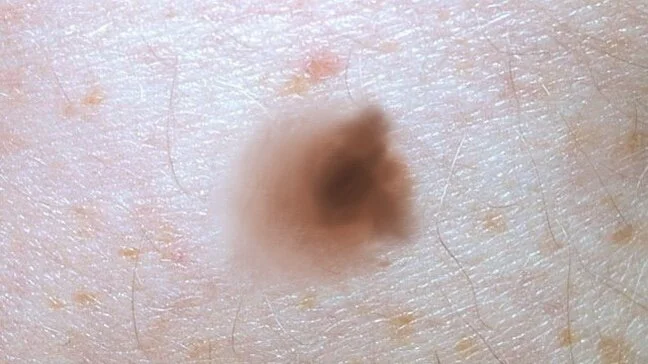
Introducing the ABCDEs of Melanoma
Melanoma prognosis is dramatically improved with earlier detection, so self skin checks monthly is an excellent way to assist. Distinguishing between benign and malignant lesions can seem like a daunting task to patients. The ABCDEs of melanoma is a teaching tool used in the hopes of making this process easier. While not every mole will be perfect in every respect using these tools should make it easier to notice spots that require attention by your dermatologist.
Asymmetry
A is for Asymmetry: Look for moles spots that look unbalanced with respect to shape or color.
Border Irregularity
B is for Border: The border should be well defined and smooth. Smudged borders or jagged borders are irregular.
Color Variation
C is for Color: Even colors are good, and preferably on the lighter end of the spectrum. Multiple color tones, jet black hue, reds, whites are worrisome features.
Diameter > 6mm
D is for Diameter: Congenital moles (present from birth) may naturally be larger than 6mm but for acquired moles we start to look at those larger than 6mm with more suspicion.
Evolution
E is for Evolution: Most melanomas will be a brand new spot or a changing spot. Watch for any changes in color, shape, size…etc.
Introducing the Concept of the “Ugly Duckling”
If the ABCDEs of melanoma felt too technical or intimidating then consider a simplified approach such as using the concept of the Ugly Duckling. Your brain is pretty good at picking out patterns. It will help you identify the spots that don’t belong even if you arrived there without any technical analysis.
How and When to Look

Self Skin Check Strategy
MONTHLY FREQUENCY
I tell patients to consider self skin checks as your insurance policy for melanoma. You hope you never get one, but if you do, you want to be the first one to find it during your monthly self skin check rather than wait for it to be found on an annual routine exam. Because as we stated above the earlier they are detected the better the prognosis.
PARTICULAR ATTENTION TO NEW OR CHANGING SPOTS
I recommend that patients take a few minutes before or after a shower once a month and do a deliberate self skin check. Use the tools we discussed above with particular attention to anything new or changed from previous exams. When in doubt, seek the opinion of your doctor.
CHECK ALL AREAS
Remember that melanoma can occur even where the sun doesn’t shine. So remember to check all areas of the body including the buttocks, genitalia, bottom of the feet, web of the toes, armpits, finger and toenails etc. Using a handheld mirror can help you see places you are not flexible enough to see. Consider asking a spouse or family member to look at your back and scalp.
NON-MELANOMA SKIN CANCERS:
Non-melanoma skin cancers such as basal cell carcinoma and squamous cell carcinoma occur in heavily sun damaged areas most frequently. If you have already had one skin cancer you are at significantly increased risk of another.
Basal cell carcinoma is slow but progressive in its growth. It may initially present as a non-healing wound. Or as a spot that bleeds spontaneously. If neglected it can cause local destruction.
Squamous Cell Carcinoma typically presents more quickly. It may be a rapidly growing and painful bump.
Review this resource from the American Academy of Dermatology for more information.